Understanding what ‘risk’ means
Understanding what ‘risk’ means

- What does ‘risk’ mean?
‘Risk’ is the likelihood that something might happen.
A ‘risk factor’ is something that increases the chance of developing a condition.
Myeloma risk is the likelihood that the disease will progress (get worse) or become resistant to particular treatment (also known as refractory disease).
- What are the general risk factors for developing multiple myeloma?
The general risk factors for developing multiple myeloma include:
- Age – being 65 years or older increases risk
- Sex – men have a slightly increased risk
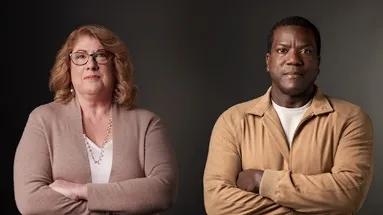
- Race – studies have shown that myeloma is more common in African Americans compared with White Americans
- Family history – having a sibling or parent with myeloma increases risk
- Body weight – being overweight or obese increases risk
- Having other plasma cell disorders increases risk
- How is risk status assessed in multiple myeloma?
In myeloma, staging is a way to help to classify risk status. Myeloma is staged using a scale known as the International Staging System (ISS). This scale uses results from two blood tests, beta-2 microglobulin and albumin level, and classifies risk status as stage I, stage II, or stage III. A higher number stage means a more advanced stage disease.
The Revised International Staging System (R-ISS) also incorporates the blood levels of an enzyme called lactate dehydrogenase (LDH) and genetic changes in the myeloma cells.
- Which features are considered ‘high risk’ for multiple myeloma?
In myeloma, risk status is described as ‘standard’ or ‘high’. The risk status that is assigned can depend on the results from the R-ISS scale, or whether your DNA has any changes in its structure – these are called chromosomal abnormalities.
Standard-risk features include:
- Having R-ISS stage I/II myeloma
- Having the chromosomal abnormalities t(11;14) or t(6;14)
High-risk features include:
- Having R-ISS stage III myeloma
- Having any of the chromosomal abnormalities del(17p), t(4;14), t(14;16), t(14,20), gain1q, p53 mutations
Note: Scientists use some abbreviations to describe alterations to DNA. ‘t’ means ‘translocation’, and it’s when parts of your DNA swap with each other. ‘del’ means deletion, and it’s when parts of your DNA are removed. ‘Gain’ is when your DNA gains additional parts. Changes to DNA are common, but some can have effects that mean myeloma can be high risk.
- How does treatment vary according to risk?
The type of treatment given for myeloma can vary based on factors including fitness level, other health conditions, how well your organs are functioning, previous medical treatments, and risk status. Treatments may also differ for patients with other conditions relating to myeloma, such as plasmacytomas [Hyperlink to new page titled “Uncommon conditions associated with multiple myeloma: Plasmacytoma and amyloidosis] or plasma cell leukemias.
People with newly diagnosed multiple myeloma who have higher risk may be given more medications to treat their disease. A drug that you take for a long period of time (often months or years) called maintenance therapy may also be different depending on whether you have standard-risk or high-risk myeloma.
Questions that might be useful for discussions with your healthcare team
It might be helpful to talk to your healthcare team about your risk status and factors that contribute to risk. The following questions might help you better understand your risk status and how it might affect your treatment:
- What type of chromosomal abnormality do I have and how will that affect my treatment options?
- How does my overall health affect my treatment options?
- What is my risk status for progression and what does it mean?
- Can you explain my pathology and blood test results?